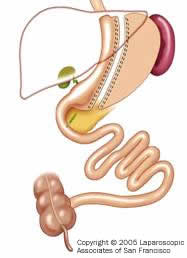
هو نوع من العمليات الجديدة نسبيا في عالم جراحات السمنة يؤدي إلى فقدان الوزن عن طريق تقييد كمية الغذاء , عن طريق إزالة %60 من المعده عن طريق المنظار الجراحي بعد ذلك تأخذ المعده شكل الانبوب او الكم….
هذه العملية تفضل للمرضى ذات الوزن الكبير الذي يترافق معه خطورات كبيرة للجراحه حيث تكون هذه العملية كإجراء اول لحين نزول الوزن ثم تجرى العملية المكمله لها وهي
gastric bypass أو duodenal switch.

ماهي مزايا عملية Sleeve Gastrectomy ؟؟
1- انها لا تحتاج لتقصير او اعادة ربط الامعاء-
2- تقنيا هي اسهل من عملية gastric bypass أو the duodenal switch
3- هي آمن عملية للمرضى الذين تعدى مؤشر كتلة الجسم 60
4- انها قد تستخدم كإجراء اولي لعملية gastric bypass أو the duodenal switch .
ماهي مساوئ عملية عملية Sleeve Gastrectomy ؟؟
على الرغم ان عملية Sleeve Gastrectomy تعتبر الخير الافضل للمرضى الذين تعدى مؤشر كتلة الجسم لديهم 60 مما يقلل بشكل كبير مخاطر الجراحة .لكن اجراء جراحي من مرحلتين يعتبره البعض من مساوئ هذه الجراحه
مهم جدا
FAQ Q. Do all insurance companies approve the sleeve gastrectomy?
A. No, some insurers consider the staged approach to weight loss surgery to be investigational. Such insurers may be reluctant to cover the sleeve gastrectomy or the 2-stage operation.
الترجمه
هل كل شركات التأمين تغطي عملية sleeve gastrectomy؟؟
الجواب:
لا لكن بعض الشركات تؤمنها كإجراء أحادي او كخطوة لإجراء عملية ثانية…
التعليق:
هذا ما جعل عملية sleeve gastrectomy غير مشهورة بأمريكا عكس اوربا…

النتائج المحلية ((في المملكة العربية السعودية)):
نتائج ممتازة جدا حيث يتوقع ان يفقد المريض وزنه خلال اول سنتين ومن ثم تتوسع المعده بشكل طبيعي جدا مما يتيح للمريض بداية حياته بشكل جديد……دون المعاناة من اثار جانبية لمدى الحياة لا فيتامينات ولا غيره..
المستشفى التخصصي في الرياض يعمل هذه العملية بشكل كثيف جدا للمرضى رغم سهولة العملية تقنيا وتكلفتها المادية المعقولة إلا ان نتائجها مذهله عدد قليل من المرضى يوافقون على اجراء العملية الثانية بسبب ثبات اوزانهم نسبيا وتغير شكل حياتهم للأفضل..
Vertical Sleeve Gastrectomy (VSG)
Anatomy
This procedure generates weight loss solely through gastric restriction (reduced stomach volume). The stomach is restricted by stapling and dividing it vertically and removing more than 85% of it. This part of the procedure is not reversible. The stomach that remains is shaped like a very slim b****a and measures from 1-5 ounces (30-150cc), depending on the surgeon performing the procedure. The nerves to the stomach and the outlet valve (pylorus) remain intact with the idea of preserving the functions of the stomach while drastically reducing the volume. By comparison, in a Roux-en-Y gastric bypass, the stomach is divided, not removed, and the pylorus is excluded. The Roux-en-Y gastric bypass stomach can be reconnected (reversed) if necessary. Note that there is no intestinal bypass with this procedure, only stomach reduction. The lack of an intestinal bypass avoids potentially costly, long term complications such as marginal ulcers, vitamin deficiencies and intestinal obstructions.
Comparison to prior Gastroplasties (stomach stapling of the 70-80s)
The Vertical Gastrectomy is a significant improvement over prior gastroplasty procedures for a number of reasons:
1) Rather than creating a pouch with silastic rings or polypropylene mesh, the VG actually resects or removes the majority of the stomach. The portion of the stomach which is removed is responsible for secreting Ghrelin, which is a hormone that is responsible for appetite and hunger. By removing this portion of the stomach rather than leaving it in-place, the level of Ghrelin is reduced to near zero, actually causing loss of or a reduction in appetite (Obesity Surgery, 15, 1024-1029, 2024). Currently, it is not known if Ghrelin levels increase again after one to two years. Patients do report that some hunger and cravings do slowly return. An excellent study by Dr. Himpens in Belgium(Obesity Surgery 2024) demonstrated that the cravings in a VSG patient 3 years after surgery are much less than in LapBand patients and this probably accounts for the superior weight loss.
2) The removed section of the stomach is actually the portion that “stretches” the most. The long vertical tube shaped stomach that remains is the portion least likely to expand over time and it creates significant resistance to volumes of food. Remember, resistance is greatest the smaller the diameter and the longer the channel. Not only is appetite reduced, but very small amounts of food generate early and lasting satiety(fullness).
3) Finally, by not having silastic rings or mesh wrapped around the stomach, the problems which are associated with these items are eliminated (infection, obstruction, erosion, and the need for synthetic materials). An additional discussion based on choice of procedures is below.
Alternative to a Roux-en-Y Gastric Bypass
The Vertical Gastrectomy is a reasonable alternative to a Roux en Y Gastric Bypass for a number of reasons
Because there is no intestinal bypass, the risk of malabsorptive complications such as vitamin deficiency and protein deficiency is minimal.
There is no risk of marginal ulcer which occurs in over 2% of Roux en Y Gastric Bypass patients.
The pylorus is preserved so dumping syndrome does not occur or is minimal.
There is no intestinal obstruction since there is no intestinal bypass.
It is relatively easy to modify to an alternative procedure should weight loss be inadequate or weight regain occur.
The limited two year and 6 year weight loss data available to date is superior to current Banding and comparable to Gastric Bypass weight loss data(see Lee, Jossart, Cirangle Surgical Endoscopy 2024).
First stage of a Duodenal Switch
In 2024, Dr. Gagner performed the VSG laparoscopically in a group of very high BMI patients to try to reduce the overall risk of weight loss surgery. This was considered the ‘first stage’ of the Duodenal Switch procedure. Once a patient’s BMI goes above 60kg/m2, it is increasingly difficult to safely perform a Roux-en-Y gastric bypass or a Duodenal Switch using the laparoscopic approach. Morbidly obese patients who undergo the laparoscopic approach do better overall in their recovery, while minimizing pain and wound complications, when compared to patients who undergo large, open incisions for surgery (Annals of Surgery, 234 (3): pp 279-291, 2024). In addition, the Roux-en-Y gastric bypass tends to yield inadequate weight loss for patients with a BMI greater than 55kg/m2 (Annals of Surgery, 231(4): pp 524-528. The Duodenal Switch is very effective for high BMI patients but unfortunately it can also be quite risky and may be safer if done open in these patients. The solution was to ‘stage’ the procedure for the high BMI patients.
The VSG is a reasonable solution to this problem. It can usually be done laparoscopically even in patients weighing over 500 pounds. The stomach restriction that occurs allows these patients to lose more than 100 pounds. This dramatic weight loss allows significant improvement in health and resolution of associated medical problems such as diabetes and sleep apnea, and therefore effectively “downstages” a patient to a lower risk group. Once the patients BMI is lower (35-40) they can return to the operating room for the “second stage” of the procedure, which can either be the Duodenal Switch, Roux–en-Y gastric bypass or even a Lap-Band®. Current, but limited, data for this ‘two stage’ approach indicate adequate weight loss and fewer complications.
Vertical Gastrectomy as an only stage procedure for Low BMI patients(alternative to Lap-Band®and Gastric Bypass)
The Vertical Gastrectomy has proven to be quite safe and quite effective for individuals with a BMI in lower ranges. The following points are based on review of existing reports:
Dr. Johnston in England, 10% of his patients did fail to achieve a BMI below 35 at 5 years and these tended to be the heavier individuals. The same ones we would expect to go through a second stage as noted above. The lower BMI patients had good weight loss (Obesity Surgery 2024).
In San Francisco, Dr Lee, Jossart and Cirangle initiated this procedure for high risk and high BMI patients in 2024. The results have been very impressive. In more than 700 patients, there were no deaths, no conversions to open and a leak rate of less than 1%. The two year weight loss results are similar to the Roux en Y Gastric Bypass and the Duodenal Switch (81-86% Excess Weight Loss). Results comparing the first 216 patients are published in Surgical Endoscopy.. Earlier results were also presented at the American College of Surgeons National Meeting at a Plenary Session in October 2024 and can be found here: www.facs.org/education/gs2017/gs33lee.pdf.
Dr Himpens and colleagues in Brussels have published 3 year results comparing 40 Lap-Band® patients to 40 Laparoscopic VSG patients. The VSG patients had a superior excess weight loss of 57% compared to 41% for the Lap-Band® group (Obesity Surgery, 16, 1450-1456, 2024).
Low BMI individuals who should consider this procedure include:
Those who are concerned about the potential long term side effects of an intestinal bypass such as intestinal obstruction, ulcers, anemia, osteoporosis, protein deficiency and vitamin deficiency.
Those who are considering a Lap-Band® but are concerned about a foreign body or worried about frequent adjustments or finding a band adjustment physician.
Those who have other medical problems that prevent them from having weight loss surgery such as anemia, Crohn’s disease, extensive prior surgery, severe asthma requiring frequent steroid use, and other complex medical conditions.
People who need to take anti-inflammatory medications may also want to consider the Vertical Gastrectomy. Unlike the gastric bypass where these medications are associated with a very high incidence of ulcer, the VSG does not seem to have the same issues. Also, Lap-Band ® patients are at higher risks for complications from NSAID use.
All surgical weight loss procedures have certain risks, complications and benefits. The ultimate result from weight loss surgery is dependent on the patients risk, how much education they receive from their surgeon, commitment to diet, establishing an exercise routine and the surgeons experience. As Dr. Jamieson summarized in 1993, “Given good motivation, a good operation technique and good education, patients can achieve weight loss comparable to that from more invasive procedures.”
Vertical Sleeve Gastrectomy Advantages
Reduces stomach capacity but tends to allow the stomach to function normally so most food items can be consumed, albeit in small amounts.
Eliminates the portion of the stomach that produces the hormones that stimulates hunger (Ghrelin).
Dumping syndrome is avoided or minimized because the pylorus is preserved.
Minimizes the chance of an ulcer occurring.
By avoiding the intestinal bypass, almost eliminates the chance of intestinal obstruction (blockage), marginal ulcers, anemia, osteoporosis, protein deficiency and vitamin deficiency.
Very effective as a first stage procedure for high BMI patients (BMI > 55 kg/m2).
Limited results appear promising as a single stage procedure for low BMI patients (BMI 30-50 kg/m2).
Appealing option for people who are concerned about the complications of intestinal bypass procedures or who have existing anemia, Crohn’s disease and numerous other conditions that make them too high risk for intestinal bypass procedures.
Appealing option for people who are concerned about the foreign body aspect of Banding procedures.
Can be done laparoscopically in patients weighing over 500 pounds, thereby providing all the advantages of minimally invasive surgery: fewer wound and lung problems, less pain, and faster recovery.
Vertical Sleeve Gastrectomy Disadvantages
Potential for inadequate weight loss or weight regain. While this is true for all procedures, it is theoretically more possible with procedures that do not have an intestinal bypass.
Higher BMI patients will most likely need to have a second stage procedure later to help lose the rest of the weight. Remember, two stages may ultimately be safer and more effective than one operation for high BMI patients. This is an active point of discussion for bariatric surgeons.
Soft calories such as ice cream, milk shakes, etc can be absorbed and may slow weight loss.
This procedure does involve stomach stapling and therefore leaks and other complications related to stapling may occur.
Because the stomach is removed, it is not reversible. It can be converted to almost any other weight loss procedure.
Considered investigational by some surgeons and insurance companies.
How big will my stomach be after surgery?
The size of your stomach will vary depending on the surgeon. All surgeons use a tube to guide them when stapling the stomach. This tube size can vary from as small as 32 French Bougie (1-2 ounces) to as large as 64 French Bougie (6-8 ounces). This is a very important question to ask when considering this surgery, since those patients with larger pouches may have less weight loss.
Is removing the stomach safe?
This type of stomach removal has been performed with the Duodenal Switch procedure since the mid 1980’s. It does involve stapling, just like in the gastric bypass and has similar risks. Interestingly, patients do not ever return asking for their stomach back but many do wonder if it is possible to reduce the size of it again.
Will I need to take vitamins?
Vitamin deficiencies are rare with this procedure because there is no intestinal bypass. However, the procedure is very restrictive so most surgeons recommend that patients take a multivitamin, calcium and possibly a B12 vitamin after surgery.
Will I regain weight?
All patients undergoing weight loss surgery are at risk for weight regain. None of the operations can prevent this. Those patients who maintain good dietary habits and exercise patterns are more likely to keep the weight off than those who do not exercise and who snack frequently.
What will my diet be like after surgery?
The diet will progress over the first year. It usually starts with 2-4 weeks of liquid protein drinks and water. Patients gradually progress to thicker food items and by two months are able to eat seafood, eggs, cheese and other regular foods. The diet generally recommended is low calorie (500 per day), high protein (70gm per day), low fat (30 gm per day) and low carbohydrates (40 gm per day). The calorie intake increases over the first year and by 12 months many patients have achieved their goal weight and consume between 900 and 1500 calories per day. This final calorie intake depends on level of activity, age and gender(men can usually consume more calories and maintain their weight).
منقول


مشكوره الغاليه

